

Close


If you’re trying to conceive, you’ve likely encountered discussions about the importance of “egg quality.” However, it’s essential to recognize that while egg quality is significant, follicle quality plays a pivotal role in the conception process, and it’s something a woman can actively influence. In this blog post, we’ll explore the concept of follicle quality and its impact on fertility. We’ll delve into the factors that affect follicle health and the strategies you can employ to optimize it.
Whether you’re embarking on your TTC journey or have been actively trying to conceive for some time, understanding the role of follicle quality is paramount to maximizing your chances of pregnancy success.
Let’s delve deeper into this crucial aspect of fertility!
Egg quality and follicle quality are closely related but distinct concepts in female reproductive health. Both are critical for successful conception and pregnancy, but they refer to different aspects of the reproductive process.
Egg quality encompasses the health and viability of the oocyte (egg cell), including its genetic integrity and capacity for fertilization, embryonic development, and successful pregnancy. Meiosis, the specialized cell division process responsible for producing gametes (egg and sperm cells), significantly influences the quality of an egg.
Factors Affecting Egg Quality:
Indicators of Poor Egg Quality:
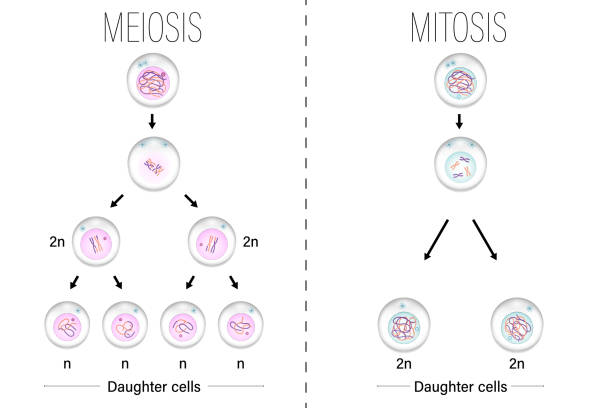
Follicle quality pertains to the health and functionality of the entire ovarian follicle, comprising the oocyte (egg) along with the surrounding granulosa and theca cells. These cells facilitate the egg’s development and maturation by producing hormones and supplying nutrients. During the initial stages of ovarian follicle development, the granulosa and theca cells undergo proliferation via mitosis.
Factors Affecting Follicle Quality:
Indicators of Poor Follicle Quality:
| Egg Quality | Follicle Quality | |
|---|---|---|
| Focus | Health and viability of the egg cell | Health and functionality of the entire follicle |
| Components | Genetic material, mitochondrial function, ability to fertilize and develop | Oocyte, granulosa cells, theca cells, hormonal support |
| Primary Influences | Age, genetic integrity, oxidative stress, hormonal balance | Hormonal environment, blood supply, inflammation, lifestyle factors |
| Indicators | High miscarriage rate, difficulty conceiving, aneuploidy | Irregular menstrual cycles, anovulation, low antral follicle count, poor hormonal response |
| Impact on Fertility | Directly affects embryo development and pregnancy success | Supports egg maturation and readiness for ovulation |
In summary, while egg quality focuses on the viability and genetic integrity of the oocyte, follicle quality encompasses the overall environment and support system that nurtures the egg. Both are crucial for successful conception and maintaining a healthy pregnancy.
Follicle quality is a crucial consideration when it comes to trying to conceive (TTC). While egg health is often discussed, follicle quality plays an equally significant role and is something a woman can actively influence. In this section, we’ll delve deeper into the various factors that affect follicle quality.
Age
Age remains a primary determinant of follicle quality. As women age, the quality and quantity of their follicles typically decline, posing challenges to conception. Diminished follicle quality raises the likelihood of chromosomal abnormalities, which can lead to miscarriage or congenital disabilities.
Despite age-related declines, research indicates that follicle quality can be improved irrespective of age. Embracing a balanced diet and engaging in regular physical activity can notably enhance follicle quality. Reducing exposure to environmental pollutants and refraining from smoking are also beneficial. Certain supplements and medications, such as CoQ10 and DHEA, have demonstrated effectiveness in enhancing follicle quality, particularly in older women. While age-related changes pose obstacles, proactive measures can be taken to enhance the likelihood of conception.
Lifestyle Factors
In addition to age, various lifestyle factors influence follicle quality. A woman’s diet, exercise regimen, smoking habits, and alcohol consumption all contribute to follicle health. Consuming a nutritious diet rich in antioxidants, healthy fats, and protein can optimize follicle quality. Conversely, excessive alcohol intake and smoking can detrimentally affect follicle health. Exercise is another crucial factor, with moderate physical activity positively impacting fertility. However, excessive or intense exercise may have adverse effects.
It’s essential to recognize that even minor lifestyle adjustments can significantly enhance follicle quality, underscoring the importance of making healthy choices for overall reproductive well-being.
Medical issues can have a considerable influence on fertility and egg quality. Polycystic ovary syndrome (PCOS) and endometriosis are two of the most common medical problems that can adversely affect egg and follicle quality.
PCOS, a hormonal disorder, can disrupt ovulation, resulting in irregular periods and decreased fertility. This can also impact egg and follicle quality, as the hormones that regulate ovulation play a role in egg maturation.
Endometriosis is a medical condition in which tissue similar to the lining of the uterus grows outside the uterus. Inflammation and scarring can occur, which may result in a reduction in ovarian function and a deterioration in the quality of eggs produced.
Working with a functional nutrition practitioner specializing in fertility and hormone health is essential to optimizing your reproductive health and improving your chances of conception.
Functional nutrition is an approach that looks at the root cause of health issues and aims to optimize health through targeted nutrition interventions. Functional nutrition can be crucial in enhancing reproductive health and increasing the probability of conception, particularly for women with conditions such as endometriosis and PCOS. Functional nutritionists can help identify dietary triggers contributing to symptoms such as inflammation and hormonal imbalances.
They can then recommend nutrient-dense foods and supplements that support reproductive health, such as omega-3 fatty acids, antioxidants, and vitamin D. By addressing underlying imbalances through a functional nutrition approach, women with PCOS and endometriosis can potentially improve their egg and follicle quality, supporting their chances of conceiving.
Environmental toxins are a growing concern for reproductive health and fertility. Exposure to chemicals, pesticides, and pollutants from air, water, and food sources can negatively impact fertility. Studies have shown that exposure to toxins such as bisphenol A (BPA), phthalates, and heavy metals can result in lower ovarian reserve and reduced fertility.
Reducing exposure to these toxins is crucial to protect reproductive health, including preserving egg and follicle quality. Simple steps like using natural cleaning products, filtering drinking water, and choosing organic foods can help reduce exposure to environmental toxins and improve your chances of conception.
Understanding the factors that affect egg and follicle quality may help you take steps to improve your reproductive health and increase your chances of conceiving. The following section will discuss how to assess egg and follicle quality to determine the best course of action in your TTC journey.
Understanding the factors that impact egg and follicle quality is crucial in optimizing fertility. However, it can be challenging to recognize the signs of poor egg quality and follicle development. In the following section, we will explore the indicators of poor egg and follicle quality and their potential impact on conception.
Poor egg quality and follicle health can present challenges for couples trying to conceive. While these issues may not always manifest with overt symptoms, certain signs can signal underlying problems.
These include irregular periods, abnormal bleeding, changes in cervical fluid, failed IVF cycles, and miscarriage. These symptoms may stem from various factors, such as hormonal imbalances or age-related declines in egg and follicle health.
If you notice any of these signs, consulting with a qualified healthcare provider or hormone health specialist is crucial. In the sections that follow, we will explore strategies to improve egg and follicle quality and increase the chances of successful pregnancy.
It is essential to discuss any signs of poor egg health and follicle quality with a healthcare provider or a functional nutrition provider. These signs can be indicative of underlying fertility issues and may require further testing and treatment.
Now that you know the signs that may indicate poor egg and follicle health, exploring ways to improve it is essential. In the next section, we will discuss various methods to enhance egg and follicle quality and boost the chances of conception. These include strategies such as diet and nutrition, exercising, managing stress, taking supplements, and more.
Enhancing follicle quality is a crucial aspect of optimizing fertility and increasing the likelihood of conception. While the process of egg development begins before birth and is largely determined by genetic factors, there are steps individuals can take to support follicle quality, thereby influencing egg health.
Here are some strategies to consider:
By incorporating these lifestyle and functional nutrition strategies into your daily routine, you can take proactive steps to support follicle health and enhance your chances of conceiving. Consulting with a healthcare provider or fertility specialist can provide personalized guidance tailored to your unique needs and circumstances, further optimizing your reproductive health journey.
It Starts With An Egg
If you’re trying to conceive, one resource that may support you on your fertility journey is It Starts With An Egg by Rebecca Fett.
This robust book is packed with research-backed strategies to help improve egg quality and boost your chances of conceiving. It covers all topics related to reproductive health, including the impact of diet and nutrition, the benefits of taking supplements, the role of exercise, and lifestyle factors that can influence egg and follicle quality.
It’s no wonder why so many people turn to this book as a guide to optimizing their fertility and increasing their chances of getting pregnant.
It Starts With An Egg: A Few Key Points
| Strategy | Action | Research |
| Remove environmental toxins | Avoid exposure to chemicals, pesticides, and pollutants | Reducing exposure to environmental toxins can help preserve egg quality. |
| Diet and nutrition | Consume a diet rich in antioxidants, healthy fats, and protein | Studies have shown that a diet rich in antioxidants, healthy fats, and protein can improve egg quality. |
| Supplements | Take CoQ10 and omega-3 fatty acids | CoQ10 is a powerful antioxidant that may help improve egg quality, while omega-3 fatty acids may improve embryo quality. Studies have shown that CoQ10 supplementation can improve pregnancy rates and reduce the risk of chromosomal abnormalities. |
| Exercise | Engage in regular moderate exercise | Regular moderate exercise has been shown to improve fertility and egg quality. However, excessive exercise can have the opposite effect. |
| Stress management | Practice stress-reducing activities such as yoga or meditation | High levels of stress can have a negative impact on fertility and egg quality. Practicing stress-reducing activities has been shown to improve reproductive outcomes. |
| Acupuncture | Try acupuncture to improve blood flow and reduce stress | Acupuncture may improve blood flow to the reproductive organs and reduce stress, potentially improving fertility and egg quality. |
It is important to keep in mind that while supplements may be beneficial, they should not be the only means for improving egg development and follicular health. It’s essential to prioritize a nutritious diet, regular physical activity, effective stress management, and limiting exposure to harmful environmental toxins.
Working with a functional nutrition practitioner is essential to ensure that you are taking the right supplements in the right amounts. A functional nutrition practitioner can help you identify which supplements are best for your individual needs and health status and help you create a personalized supplement protocol. A practitioner can also keep track of your advancements and modify your supplement regimen if necessary. Collaborating with a professional can guarantee that the supplements you are taking are both safe and efficient.
While several lifestyle changes and supplements may support healthy egg and follicular health, sometimes medical interventions may be part of your journey to achieve a successful pregnancy. The following section will discuss some medical interventions available for individuals with poor egg quality.
If you are struggling with poor egg quality, several medical interventions may support your chances of conceiving. Here are a few options to consider:
It is crucial to bear in mind that these medical interventions may not be appropriate for all individuals, and it is necessary to have a conversation about your choices with a qualified healthcare provider or fertility specialist.
If you have been diagnosed with poor egg quality or are experiencing fertility issues, you may be wondering what options are available to improve your chances of conceiving. While medical interventions such as ovarian stimulation medications and IVF with pre-implantation genetic testing can be effective, there are also functional nutrition approaches that can support your reproductive health. In the next section, we will explore how working with a functional nutrition practitioner can help improve egg quality and fertility.
Functional nutrition takes a comprehensive and holistic approach to health and wellness. Its goal is to identify and address the underlying causes of health issues instead of just treating the symptoms. Functional nutrition takes into account each person’s specific needs and challenges when it comes to fertility and creates a customized plan to promote reproductive health.
Working with a functional nutrition practitioner can significantly enhance egg quality through various means. These experts can assess your dietary patterns, identify nutritional deficiencies, and develop a personalized nutrition plan aimed at optimizing reproductive health. Additionally, they can address underlying health issues that may affect fertility, such as gut imbalances, inflammation, or hormonal imbalances, using a holistic approach that encompasses diet, lifestyle adjustments, and supplementation.
Improving egg quality is vital for both natural conception and those utilizing reproductive technologies like IVF, where the quality of eggs and follicles is a critical factor in the success of fertilization, implantation, and maintaining a healthy pregnancy. By collaborating with a functional nutrition practitioner, individuals seeking to conceive can greatly improve their reproductive health and increase their chances of a successful conception.
A functional nutrition approach to fertility tailors strategies to each individual’s needs, addressing underlying health imbalances that could impact reproductive outcomes. Research supports that a personalized nutrition strategy not only addresses deficiencies but also optimizes overall nutrient intake, thereby enhancing fertility. For those undergoing assisted reproductive technologies such as IVF, recent studies underscore the importance of high-quality eggs and follicle health in increasing the likelihood of successful treatment outcomes. By integrating a functional nutrition approach, individuals may significantly boost their prospects for success with fertility treatments.
Working with a functional nutrition practitioner and adopting fundamental lifestyle changes can improve your egg quality and increase your chances of conceiving naturally or through reproductive technologies. Let’s recap the key takeaways for improving egg quality and encourage seeking medical advice if you’re experiencing fertility issues.
When trying to conceive, egg quality and follicle health are crucial factors that can significantly affect the chances of successful conception. It is essential to consider various lifestyle factors impacting egg quality, such as diet, exercise, smoking, and alcohol consumption.
Additionally, medical conditions like PCOS and endometriosis and exposure to environmental toxins can also affect egg health and follicle quality. However, various strategies can help improve fertility, such as removing ecological toxins, following a nutrient-dense diet, incorporating supplements like CoQ10 and omega-3 fatty acids, regular exercise, stress management, and acupuncture.
Seeking the guidance of a functional nutrition practitioner can also help support fertility and improve follicle health. In conclusion, those experiencing fertility issues should not hesitate to seek qualified advice and explore various strategies for improving egg and follicle quality to optimize their chances of successful conception and pregnancy.
Disclaimer:
The information provided on this blog is for educational and informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. The content on this blog is not meant to replace professional medical advice or to be used to prevent, diagnose, or treat any disease or illness. Reliance on any information provided by this blog is solely at your own risk.
Sign up today and receive your FREE Resource Bundle to support your journey towards hormone health, fertility, gut wellness, cycle wisdom, and holistic nutrition!