

Close

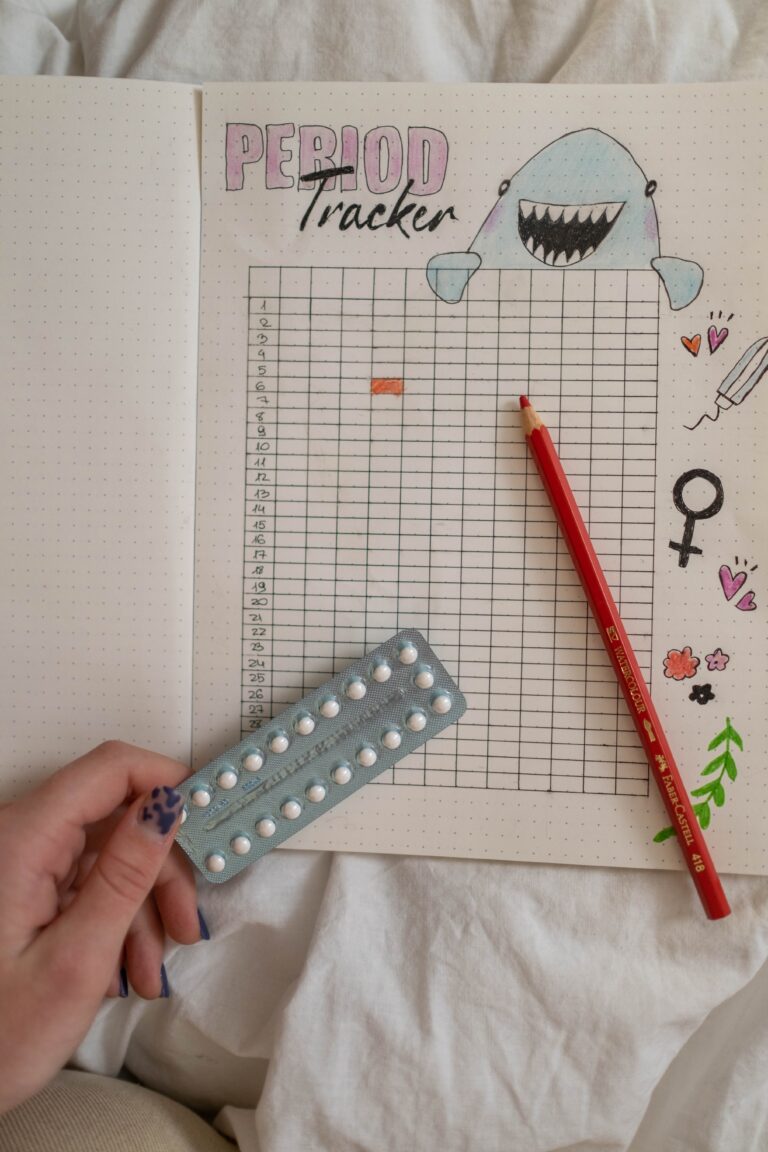
Exploring the connection between fertility awareness and birth control can seem overwhelming given the myriad of contraception methods available. It’s like navigating a complex menu of options for your reproductive and sexual health. Let’s delve into this topic together and find the strategies that best suit your body, clarifying any confusion and expanding your understanding.
Fertility awareness methods entail tracking the menstrual cycle and understanding peak fertility periods. Hormonal birth control, on the other hand, uses synthetic hormones to prevent ovulation and pregnancy.
It’s important to understand the differences between these two contraceptive approaches, as they significantly impact your body and overall health. In this blog post, we’ll explore the ins and outs of fertility awareness and hormonal birth control, including the benefits and drawbacks of each.
So whether you’re trying to conceive, looking for a natural approach to birth control, or simply curious about your options, keep reading to learn more.
Fertility awareness is a method of contraception that involves tracking your menstrual cycle and ovulation to determine when you are most likely to be fertile. This method is based on the fact that there are only a handful of days during your cycle when you are actually fertile and can become pregnant. By identifying when you are fertile, you can either avoid sexual intercourse or use a barrier method of contraception, such as condoms, during that time if you are interested in avoiding pregnancy.
One of the benefits of fertility awareness is that it is a natural method of contraception that does not involve the use of hormones or devices. It can also empower individuals to understand their menstrual cycles and fertility patterns. However, it is essential to note that fertility awareness requires consistent and accurate cycle tracking, which may be unsuitable for some.
Different fertility awareness methods include tracking your basal body temperature, monitoring changes in cervical mucus, and understanding your body’s signals related to hormone shifts and changes. Basal body temperature tracking involves measuring your temperature every morning to detect a slight increase that occurs after ovulation. Monitoring cervical mucus entails tracking changes in vaginal discharge throughout your cycle. Other signs that a person may monitor are changes in cervical position, mood, sleep patterns, libido, and more.
While fertility awareness can be an effective method of contraception, it may take more time to learn than using other methods, such as hormonal birth control or barrier methods. It is essential to carefully consider your options and explore speaking with a qualified fertility awareness educator as you consider engaging with fertility awareness based methods.
Understanding the differences between fertility awareness and hormonal birth control is essential in deciding which method of contraception is suitable for you. While fertility awareness methods entail monitoring your menstrual cycle and identifying fertile days, hormonal birth control uses synthetic hormones to prevent pregnancy. Let’s take a closer look at the pros and cons of fertility awareness methods.

Hormonal birth control is a popular contraceptive option for many people. It works by altering the body’s hormonal balance to prevent ovulation, which means the release of an egg from the ovaries. Hormonal birth control can come in various forms, such as pills, patches, injections, and implants.
One of the main benefits of hormonal birth control is its high effectiveness in preventing pregnancy when used correctly. Hormonal birth control prevents pregnancy by stopping the hormonal fluctuations regulating the menstrual cycle. This prevents ovulation and can also alter the thickness of cervical mucus to prevent sperm from reaching the egg. It’s important to note that hormonal birth control does not regulate cycles but stops people from having natural cycles altogether.
Like any other medication, hormonal birth control has its drawbacks. Common side effects include mood changes, headaches, weight gain, and decreased libido. It is also important to note that hormonal birth control does not protect against sexually transmitted infections (STIs).
When considering hormonal birth control, it’s important to discuss it with your healthcare provider to determine which method is right for you. Some types of hormonal birth control may be more suitable for specific individuals based on factors such as medical history and lifestyle.
Overall, while hormonal birth control can be an effective and convenient form of contraception, weighing its benefits and drawbacks before deciding if it’s the right choice for you is crucial.
There are significant differences between fertility awareness and hormonal birth control when choosing a contraceptive method. These differences can be categorized into philosophical and lifestyle differences, effectiveness and failure rates, and health risks and side effects.
Philosophically, fertility awareness methods are based on the belief that it is possible to understand and work with the body’s natural fertility cycles. This method involves tracking and charting the menstrual cycle, basal body temperature, and cervical fluid to determine the fertile window and abstaining or using backup methods from sexual activity during this time.
On the other hand, hormonal birth control is designed to stop ovulation and hormonally change the body by disrupting the natural ebb and flow of hormones involved in pregnancy. This method is not based on the body’s natural fertility cycle and can be seen as going against it.
Effectiveness and failure rates are often a point of confusion between these two methods.
Fertility awareness can be highly effective, with a failure rate of less than 1%; it requires diligent adherence to the method and careful menstrual cycle tracking. Hormonal birth control can also be effective, with a failure rate of less than 1% when used correctly.
Both fertility awareness methods and many hormone contraceptives can be prone to user error.
Health risks and side effects are other essential factors to consider when choosing between these two methods. Hormonal birth control can have potential health risks and side effects such as blood clots, high blood pressure, depression, and decreased libido. Fertility awareness, while natural and non-invasive, requires dedication and commitment.
Ultimately, choosing between fertility awareness and hormonal birth control comes down to personal beliefs, lifestyle factors, and health considerations. It is important to carefully consider the differences and consult a healthcare provider to determine the best method for your needs.
Choosing a contraceptive method that works best for you is an important decision that requires careful consideration. There are several factors to consider when choosing a method of contraception. These factors include personal preferences and medical history. Here are some key things to remember when deciding between fertility awareness and hormonal birth control.
First, you must discuss your options with your healthcare provider educated in both natural and pharmaceutical forms of contraception or a fertility awareness educator. These providers can offer contraception counseling and help you make an informed decision based on your needs and circumstances. They can also discuss each method’s potential health risks and side effects.
Consider your personal beliefs and lifestyle. Some people prefer a more natural approach and may find fertility awareness methods a good fit for them. Others may prefer the convenience of hormonal birth control.
Your medical history may also play a role in your decision. For example, if you have a history of blood clots, you may require a non-hormonal contraceptive method.
Remember, deciding which contraceptive method to use is personal and should be based on your individual needs and circumstances. By talking to your healthcare provider or a fertility awareness educator and carefully considering your options, you can make an informed decision that works best for you.
In conclusion, you must understand the key differences between fertility awareness and hormonal birth control to make informed decisions about your reproductive and sexual health. Fertility awareness relies on tracking ovulation and understanding one’s menstrual cycle, while hormonal birth control uses synthetic hormones to prevent pregnancy.
Both methods have their own benefits and drawbacks, and it’s important to consider personal preferences, lifestyle, and health when deciding about contraception.
Remember to talk to a certified fertility awareness educator or qualified healthcare provider about your options and make a wise decision that best suits your sexual health and overall well-being. By taking a proactive approach to contraceptive choice, you can feel empowered and in charge of your reproductive health.
Disclaimer:
The information provided on this blog is for educational and informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. The content on this blog is not meant to replace professional medical advice or to be used to prevent, diagnose, or treat any disease or illness. Reliance on any information provided by this blog is solely at your own risk.
Sign up today and receive your FREE Resource Bundle to support your journey towards hormone health, fertility, gut wellness, cycle wisdom, and holistic nutrition!